Every year millions of people suffer traumatic brain injuries. Many who survive a TBI recover completely, while others suffer long-term effects. One such condition is Anosmia following a head injury.
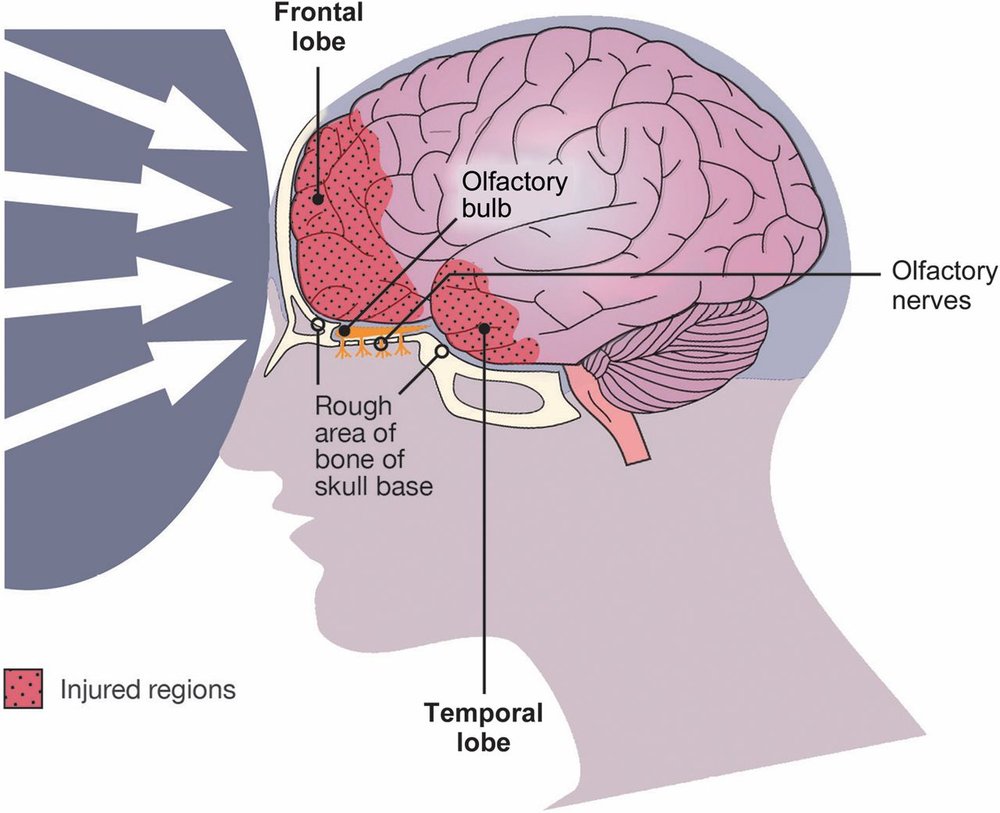
It has been found that up to 20% of patients who suffer a traumatic brain injury go on to experience olfactory dysfunction.
Olfactory dysfunction is simply any abnormal change to your ability to smell. The sense of smell, or olfaction, refers to the ability to detect and differentiate smells that you encounter so that you can determine the presence or absence of a particular scent. The sense of smell is one of our fastest senses and is directly linked to memory.
Experiencing olfactory dysfunction can have a significant impact on day-to-day life, including an impaired ability to smell, which is frequently misattributed to having a cold or lacking adequate hygiene. Despite the high prevalence of olfactory dysfunction post-TBI, treatment options in the U.S. are extremely limited and thus far untested on the effectiveness of these remedies for TBI patients.
In a systematic review that was done by Proskynitopoulos et al. it was found that 80% of the studies reviewed reported a significant association between trauma severity and olfaction. They concluded that ‘olfactory dysfunction is a prevalent but under diagnosed problem in mild traumatic brain injury’. They go on to suggest that olfactory function should be assessed when patients present with even mild traumatic brain injuries due to olfactory dysfunction being associated with a significant decrease in quality of life. The likelihood of olfactory dysfunction increases with the increased severity of the trauma.
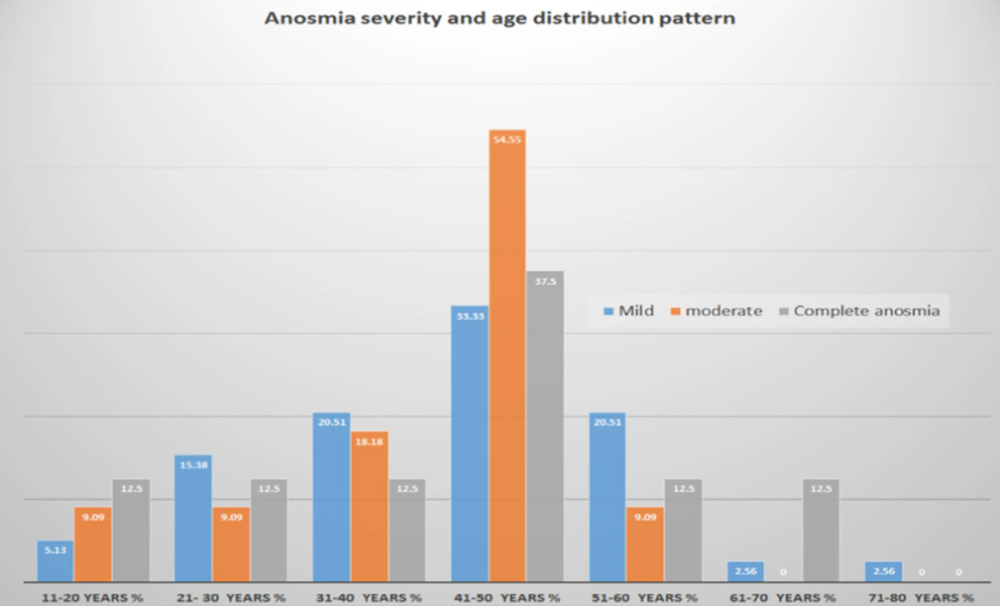
Traumatic brain injuries are classified into three categories: mild, moderate, and severe. This is based on the Glasgow Coma Scale (GCS), a common neurological scale used to determine whether the injury. And mild traumatic brain injury (MTBI) is the most common form of brain injury.
Can smell training help with recovering your smell after a brain injury?
The short answer is yes! It might seem counter-intuitive, because smell is such an involuntary process. But there’s scientific evidence that proves the efficacy of smell training for TBI patients.
In a 2019 study conducted by Robert Pellegrino et al, the effects of smell training were assessed in patients with post-traumatic smell loss. The Sniffin’ Sticks method was used to classify patients as anosmic (no smell at all) or hyposmic (significantly reduced sense of smell) and to measure changes after smell training.
What they found after 24 weeks of smell training (where smell training was performed twice daily, every day, with four odours) was that patients had an increase in test scores (Sniffin’ Sticks score), specifically in threshold and identification.
The study concluded that smell training improves olfactory performance in patients with post-traumatic smell loss and seems to be driven in part by a top-down process (central) as opposed to a bottom-up process (peripheral). This simply means that the rehabilitative benefits of smell training are realized from changes within the brain and how smell signals are received, as opposed to how smell signals are conducted from the nose.
Scientific research study proves that there is a positive, measurable correlation between the training of an individual’s sense of smell and improvement in olfactory function.
New Developments in Smell Training & Recovery
The Covid-19 pandemic introduced new challenges at both the local and international levels. It shined an especially bright light on smell loss and its effect on our quality of life. Before the pandemic, smell and taste loss were considered relatively rare symptoms, and thus not much research was done on the topic. Early research that was done on smell and taste loss, most of it was related to traumatic brain injury or noxious substances. With greater awareness of smell loss from Covid-19 and new funding from research, scientists have been studying this symptom with new vigor.
The big misconception is that smell training was created as a solution to COVID-19 smell and taste loss (or post-viral smell and taste loss), however, it is a rehabilitative exercise that has existed for quite some time. Most of its early application has been in brain trauma patients and is a valid rehabilitative therapy that can be performed safely and effectively at home.
Although there has been no identified period of time where smell training would be considered unhelpful, there is a correlation between how early patients begin smell training following their trauma, and how quickly they are able to regain their sense of smell. Simply put, the sooner smell training is undertaken, the sooner the patient will recover their sense of smell.
Undertaking an olfactory training program can be a daunting task for many patients, but it is essential to journey towards recovery.
The introduction of modified smell training is a newer form of olfaction therapy that is more effective for smell loss victims.
As a newer form of smell therapy, modified smell training is proving to be more effective for smell loss victims. Traditional smell training uses 4 different essential oils and has been found to be effective in helping these individuals. However, with modified smell training using 8-12 essential oils, the participants have seen an increase in the ability to identify odors

